Connect With Us
Blogs

Changes to the Feet During Pregnancy

Many women experience foot problems during pregnancy due to hormonal and physical adjustments in the body. Increased levels of certain hormones loosen the ligaments. This allows the arches of the feet to flatten under the added weight, which can lead to pain or changes in alignment. The extra pressure on the feet can also cause swelling, known as edema, as fluid accumulates in the lower legs and ankles. This can make shoes feel tight or uncomfortable. A shifting center of gravity often alters posture and gait, placing additional strain on the feet and ankles. Some women notice their feet become longer or wider as a result of these changes. A podiatrist can evaluate changes in arch height, swelling, or pain, and recommend orthotics or supportive footwear to improve comfort and stability. If you have foot pain related to pregnancy, it is suggested that you make an appointment with a podiatrist for a diagnosis and treatment.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with one of our podiatrists from Garnet & Carbonell, DPM, LLC. Our doctors will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions, please feel free to contact our offices located in Palmetto Bay, South Miami, and Homestead, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Care for Pregnant Women
The natural weight that pregnant women gain causes their center of gravity to be completely altered. This causes them to have a new weight-bearing stance which adds pressure to the knees and feet. As a result, pregnant women often experience severe foot pain. The two most common foot issues experienced by women in their pregnancies are edema and over-pronation. It is important for all pregnant women to learn more about how to take care of their feet so they are more comfortable during their pregnancy.
Over-pronation, which is commonly referred to as flat feet, is caused when a person’s arch flattens out upon weight bearing. This causes the person’s feet to roll inward while walking. Pregnant women often experience this due to the sudden weight they gain.
Edema, also referred as swelling in the feet, typically occurs in the later part of the pregnancy. It is the result of the extra blood accumulated in the pregnant woman’s body. The enlarged uterus puts more pressure on the blood vessels in the pelvis which causes leg circulation to slow down. This causes blood to pool in the lower extremities.
Fortunately, there are ways to treat both edema and over-pronation. Edema can be treated by elevating the foot as often as possible. Wearing proper fitting footwear will also be helpful for those with edema. A treatment method for over-pronation could be orthotics. Orthotic inserts should be designed with appropriate arch support and medial rear foot for your foot.
It is best for pregnant women to buy new shoes during the day, because this is the time where swelling is at its peak. Pregnant women also shouldn’t rush when buying shoes. It is always advised that you make sure your shoes fit properly but this is especially important during pregnancy.
If you are a pregnant woman, you should consult with a podiatrist in order to make sure your feet are healthy throughout the entirety of your pregnancy.
Let the Expert Treat Your Ingrown Toenails
Risk Factors for Sever’s Disease
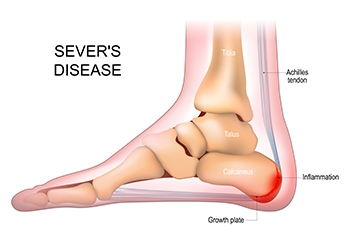
Sever’s disease is a common heel condition that affects children during growth spurts when the heel bone develops faster than the surrounding tissues. This imbalance leads to irritation at the growth plate and causes noticeable discomfort during activity. Risk factors include high-impact sports, tight calf muscles, wearing improper footwear, and having flat feet or high arches. Symptoms often begin with heel pain, tenderness, swelling, and limping after play. A podiatrist can diagnose the condition through a detailed exam and recommend conservative treatments such as stretching, footwear guidance, and activity changes to reduce strain on the heel. Early care prevents prolonged discomfort and supports healthy development. If your active child has consistent heel pain, it is suggested that you contact a podiatrist who can offer effective relief tips, ensuring your child can safely return to sporting activities.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from Garnet & Carbonell, DPM, LLC. Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Palmetto Bay, South Miami, and Homestead, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
Are Flip-Flops Damaging to My Feet?
 Looking ahead to the summer months, let’s talk flip-flops. Flip-flops tend to be an inexpensive, trendy, colorful, and easy-to-wear option for summer, but because there is little support they may be harmful to your feet. Possible injuries may include damage inflicted to the heel, typically causing severe pain. Additionally, the ligaments in the arch may be affected, which may result from improper support if continued over long periods of time. Spraining the ankle can be connected to lack of arch support, which may occur when rolled to one side. This can be alleviated when proper shoes are chosen for summer wear. There are several choices available for these “fun” shoes, including sandals with a supportive outer heel, cork soles in place of rubber soles, and solid straps that may help to hold the foot in place. Your feet will look good and, more importantly, feel good when the right shoes are chosen.
Looking ahead to the summer months, let’s talk flip-flops. Flip-flops tend to be an inexpensive, trendy, colorful, and easy-to-wear option for summer, but because there is little support they may be harmful to your feet. Possible injuries may include damage inflicted to the heel, typically causing severe pain. Additionally, the ligaments in the arch may be affected, which may result from improper support if continued over long periods of time. Spraining the ankle can be connected to lack of arch support, which may occur when rolled to one side. This can be alleviated when proper shoes are chosen for summer wear. There are several choices available for these “fun” shoes, including sandals with a supportive outer heel, cork soles in place of rubber soles, and solid straps that may help to hold the foot in place. Your feet will look good and, more importantly, feel good when the right shoes are chosen.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact one of our podiatrists from Garnet & Carbonell, DPM, LLC. Our doctors will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions, please feel free to contact our offices located in Palmetto Bay, South Miami, and Homestead, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops and Feet
Flip flops are often a popular choice of footwear for many people. Flip flops allow your feet to breathe and give your toes the freedom of movement. They are easy to slip on and can be worn with virtually any style of clothing. Flip flops, however, despite their many benefits, can be detrimental for your foot health.
Despite their comfortableness, frequently wearing flip flops can create problems in the lower body over time. Issues mainly stem from the fact that people walk differently in flip flops compared to other footwear, such as sneakers. This is due to a change in one’s natural gait, which therefore creates stress in different parts of the body while hindering the body’s natural posture. Problems can also arise in the arches and balls of the feet. Flip flops provide little to no support to these areas.
Aside from long-term problems, flip-fops can also create short-term issues as well, such as ankle sprains and blisters. Weak materials that are flexible and bendable are generally used to manufacture flip flops. These materials make its wearers prone to both tripping and injuring their ankles. Flip flops can create blisters as the material rubs against the foot. People are much more at risk for infection while wearing flip flops due to their openness. This also makes it easier to scrape and cut the foot since there is a lack of protection. If these cuts are left untreated and uncovered, the risk then becomes greater.
To prevent the aforementioned occurrences, purchase a pair of flip flops that offer significant protection. The soles of the flip flops should not be floppy, but sturdy and firm, and should not significantly bend or wiggle when lifted from the floor. Flip flops made of high-quality materials will not be affected by this problem. While higher quality flip flops may be more expensive, they will last longer and provide better protection compared to a cheaper pair. Brand name flip flops sold from a quality manufacturer are a dependable option.
There is no problem in wearing your favorite pair of flip flops so as long as you do not wear them daily or for extended periods of time. Flip flops should be replaced every 3-4 months to ensure that they provide your feet with the best protection.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
All About Toenail Fungus

Toenail fungus, medically known as onychomycosis, occurs when fungi invade the nail bed, nail plate, or surrounding tissue. The infection can develop from dermatophytes, yeasts, or molds and often begins at the edge of the nail before spreading deeper. As the fungal infection progresses, the toenail can become thick, brittle, and discolored, turning yellow, brown, or white. In some cases, the nail separates from the nail bed, causing discomfort or pain while walking or wearing shoes. Affected nails can also produce a foul odor and crumble at the edges. Fungi thrive in warm, moist environments, making feet enclosed in tight shoes or damp socks more vulnerable. A podiatrist can diagnose the type of fungal infection through visual examination and laboratory testing, helping determine the most effective course of treatment to restore healthy nail growth. If you have symptoms of toenail fungus, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment options, which may include prescribed medication.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of Garnet & Carbonell, DPM, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions please contact our offices located in Palmetto Bay, South Miami, and Homestead, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.